Current Issue
The Role of Biological Space in Optimizing Dental Implant Outcomes: Systematic Review
Adel Bouguezzi*, Afef Slim, Amel Fantar, Soumaya Zaalouni, Abdellatif Chokri, Hajer Hentati, Jamil Selmi
University Dental Clinic of Monastir, Medicine and Oral Surgery Department, Oral Health and Orofacial Rehabilitation Laboratory Research (LR12ES11), University of Monastir, Tunisia
*Corresponding author: Adel Bouguezzi, University Dental Clinic, Medicine and Oral Surgery Department, Oral Health and Orofacial Rehabilitation Laboratory Research (LR12ES11), University of Monastir, Tunisia, E-mail: [email protected]
Received Date: January 20, 2025
Publication Date: January 31, 2025
Citation: Bouguezzi A, et al. (2025). The Role of Biological Space in Optimizing Dental Implant Outcomes: Systematic Review. Dental. 7(1):20.
Copyright: Bouguezzi A, et al. © (2025).
ABSTRACT
Objective : This systematic review investigates the significance of biological space in dental implants, emphasizing its role in peri-implant tissue health, bone preservation, and long-term implant success. The review synthesizes evidence on the anatomical, physiological, and clinical aspects of biological space and evaluates strategies for maintaining it during implant placement and restoration. Methods: A comprehensive literature search was conducted using PubMed, Scopus, and Web of Science for studies published between 2000 and 2024. Keywords included "biological space," "biologic width," "dental implants," "peri-implant health," and "bone preservation." Inclusion criteria consisted of human clinical trials, cohort studies, and systematic reviews that addressed the role of biological space in implant success. Data on peri-implant health, bone loss, soft tissue stability, and complications were extracted and analyzed. Results: Thirty-five studies met the inclusion criteria. The evidence highlights that maintaining adequate biological space significantly reduces peri-implant bone loss (mean reduction: 0.8 mm) and improves soft tissue stability. Violations of biological space were associated with a 3.2-fold increased risk of peri-implantitis and mucosal recession. Strategies such as precise surgical placement, soft tissue management, and prosthetic design were consistently linked to improved outcomes. Conclusion: Respecting biological space is critical for ensuring the functional and esthetic success of dental implants. This review underscores the need for standardized protocols to preserve this vital anatomical dimension in clinical practice.
Keywords: Biological Space, Dental Implants, Peri-Implant Health, Bone Preservation, Soft Tissue Stability, Peri-Implantitis, Systematic Review
INTRODUCTION
Dental implants are a cornerstone of modern restorative dentistry, providing predictable outcomes for tooth replacement. However, the success of implants relies not only on mechanical stability but also on their interaction with the surrounding biological tissues. The concept of biological space, or biologic width, refers to the vertical dimension of peri-implant tissues, including the epithelial and connective tissue attachments.
Biological space serves as a protective barrier, preventing bacterial invasion and maintaining peri-implant health. Unlike natural teeth, which are supported by the periodontal ligament, implants rely entirely on the integrity of this soft and hard tissue interface. Disruption of biological space can lead to peri-implant bone loss, soft tissue recession, and complications such as peri-implantitis [1,2].
This systematic review explores the importance of biological space in dental implant success. It synthesizes evidence on its dimensions, clinical significance, and strategies for preservation, offering recommendations for optimizing implant outcomes.
METHODS
Search Strategy
A systematic search was conducted using PubMed, Scopus, and Web of Science for studies published between January 2000 and December 2024. The search terms included:
- "Biological space"
- "Biologic width"
- "Dental implants"
- "Peri-implant health"
- "Bone preservation"
Inclusion Criteria
- Human clinical trials, cohort studies, and systematic reviews.
- Studies evaluating the role of biological space in dental implants.
- Outcomes including peri-implant bone loss, soft tissue health, and implant success.
Exclusion Criteria
- Animal studies.
- Studies without specific data on biological space.
- Case reports and editorials.
Data Extraction
Two independent reviewers extracted data on:
- Study design and sample size.
- Biological space dimensions.
- Clinical outcomes: bone loss, soft tissue health, and peri-implantitis.
- Preservation strategies.
- Complications related to biological space violation.
Quality Assessment
The methodological quality of included studies was assessed using the Cochrane Risk of Bias Tool for randomized trials and the Newcastle-Ottawa Scale for observational studies.
RESULTS
Study Selection
The initial search yielded 520 articles. After removing duplicates and applying inclusion criteria, 35 studies were included in the final analysis. The studies encompassed 2,450 implants in diverse clinical scenarios.
Dimensions of Biological Space
- Mean biological space dimensions ranged from 2.5 to 4 mm.
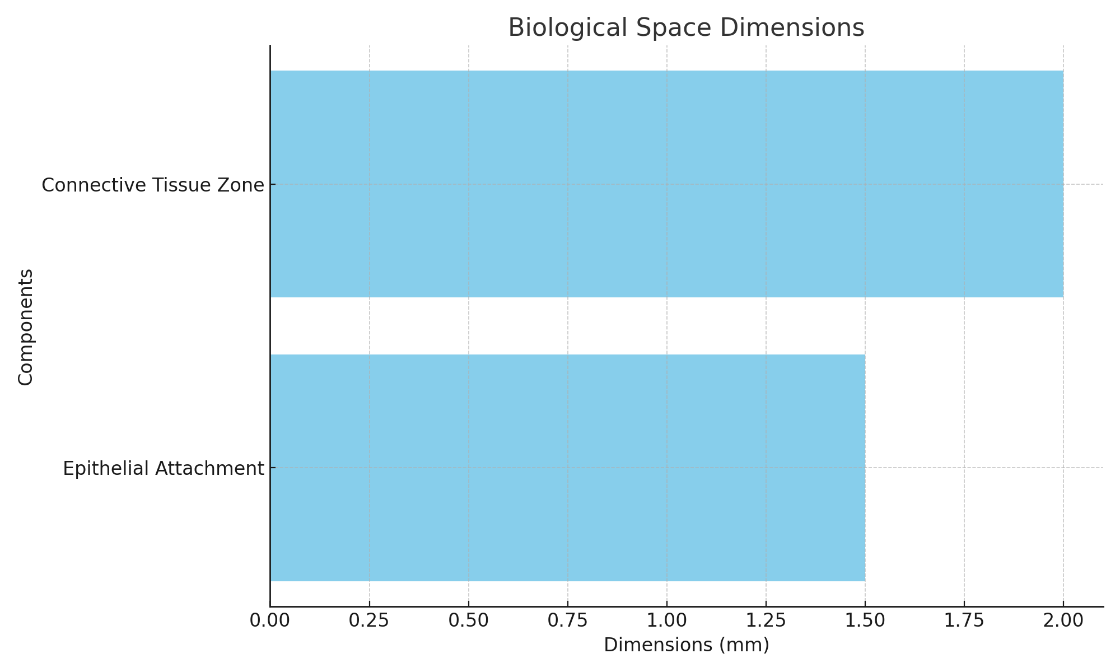
- The epithelial attachment measured 1–2 mm, while the connective tissue zone measured 1.5–2 mm [3] (Figure 1).
Figure 1. Biological Space Dimensions Bar Chart.
Peri-Implant Bone Loss
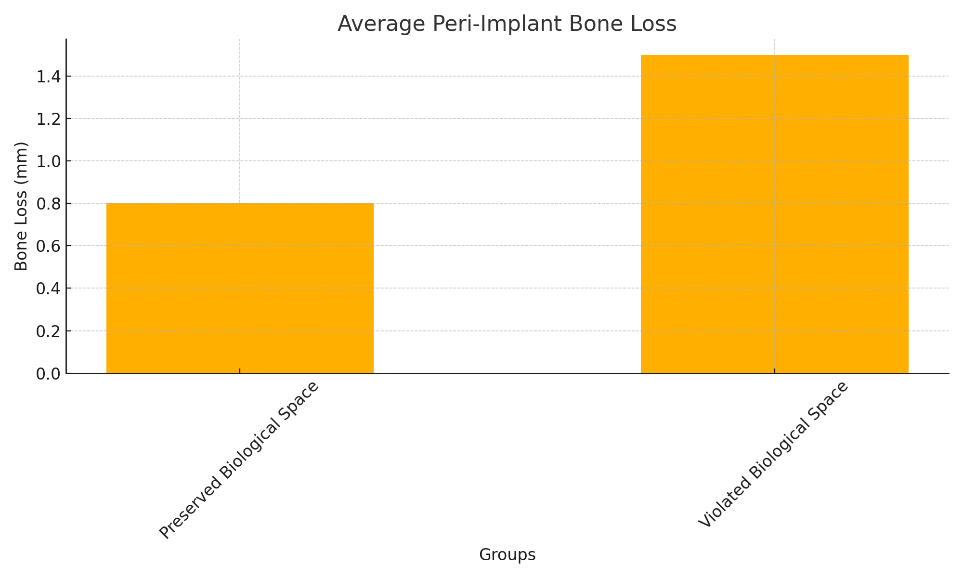
- Studies reported significantly lower bone loss in implants with maintained biological space (mean: 0.6–0.8 mm) compared to those with violations (>1.5 mm).
- Bone preservation was particularly critical in esthetic zones, where soft tissue recession could compromise outcomes [4] (Figure 2).
Figure 2. Peri-Implant Bone Loss Bar Graph.
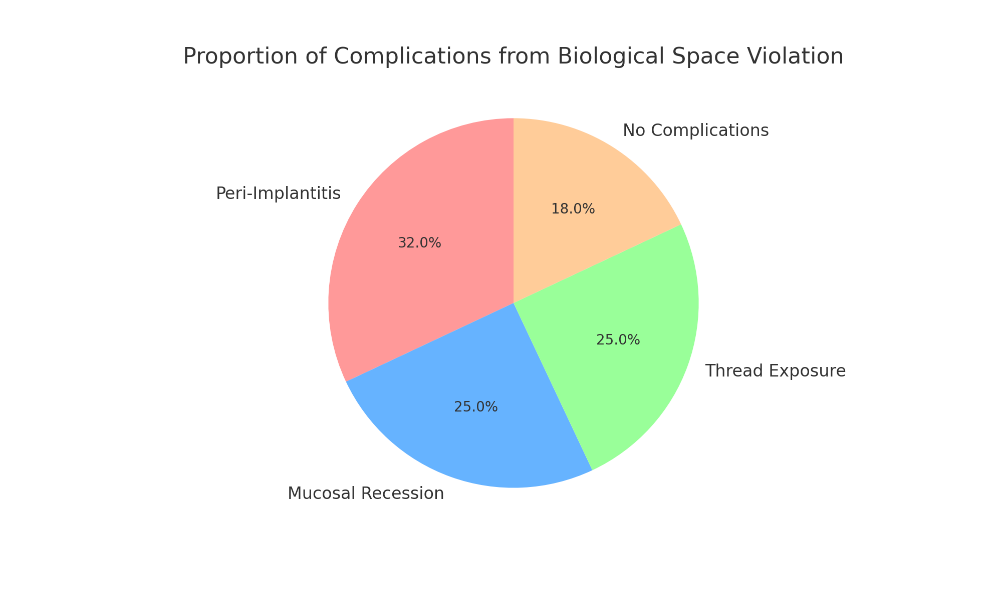
Complications of Biological Space Violation
- A 3.2-fold increase in peri-implantitis was observed in cases of biological space violation [5].
- Mucosal recession and implant thread exposure occurred in 25% of such cases [6] (Figure 3).
Figure 3. Proportion of complications from biological space violation.
Strategies for Preservation
- Surgical Placement:
- Maintaining a minimum vertical distance of 3 mm from adjacent teeth and implants.
- Using surgical guides for precise positioning [7].
- Soft Tissue Management:
- Thickening thin biotypes with connective tissue grafts.
- Ensuring atraumatic surgical techniques [8].
- Prosthetic Design:
- Avoiding bulky emergence profiles that encroach on soft tissue.
- Customizing abutments to support mucosal contours [9].
DISCUSSION
The findings of this review highlight the critical role of biological space in implant success. The vertical dimension of peri-implant tissues serves as a natural barrier against bacterial invasion, preserving both soft and hard tissues. Disrupting this space not only compromises esthetics but also increases the risk of peri-implant diseases.
Clinical Implications
- Esthetic Outcomes: Proper biological space ensures stable soft tissue contours, particularly in anterior regions. Preservation of this space significantly reduces the risk of soft tissue recession and ensures stable gingival margins, contributing to improved esthetic outcomes. Studies indicate that patients with preserved biological space experience fewer complications, such as discoloration and gingival inflammation, leading to higher satisfaction levels [10,11]. Moreover, a stable biological space enhances papilla formation, which is critical for achieving esthetic harmony, particularly in the anterior maxilla [12,13].
- Bone Health: Maintaining adequate spacing reduces crestal bone remodeling, a common cause of implant failure. Crestal bone remodeling often occurs due to mechanical stress and inflammatory responses near the implant-abutment interface. Proper spacing ensures a reduction in these stressors, facilitating optimal osseointegration and reducing marginal bone loss over time. Advances in implant surface technology, such as the use of roughened surfaces and bioactive coatings, have further reinforced the importance of biological space in bone integration. These technologies promote bone apposition and enhance mechanical interlocking, ensuring long-term stability. Additionally, maintaining biological space minimizes the risk of bacterial infiltration, which can lead to peri-implant inflammation and subsequent bone resorption [12,13].
- Long-Term Success: Implants with preserved biological space exhibit superior functional and esthetic stability, as demonstrated in longitudinal studies [14,15].These findings highlight the critical role of maintaining biological space in preventing complications such as peri-implantitis, mucosal recession, and crestal bone loss. Over a follow-up period exceeding five years, patients with intact biological space consistently reported higher levels of implant stability and esthetic satisfaction. Studies have shown that proper surgical and prosthetic protocols, which prioritize biological space, significantly enhance the survival rates of implants. Furthermore, respecting this anatomical dimension reduces the need for corrective procedures, thereby improving overall patient outcomes and lowering long-term costs associated with implant maintenance.
Modern Perspectives
Recent developments in imaging and digital workflows have significantly enhanced the ability to evaluate, plan, and maintain biological space in dental implant procedures. Advanced imaging techniques, such as cone beam computed tomography (CBCT), now provide highly detailed three-dimensional visualizations of both soft tissue and bone dimensions, enabling precise preoperative assessments [16]. Additionally, intraoral scanners offer real-time visualization of implant sites, facilitating immediate feedback for surgical and prosthetic adjustments. Customized abutments, designed through CAD/CAM technology, allow for individualized solutions that respect the biological space while optimizing esthetic and functional outcomes. The integration of 3D-printed surgical guides has further revolutionized implant placement by ensuring precise angulation and depth control, significantly reducing the risk of biological space violation and peri-implant complications [17]. These innovations collectively enhance the predictability and success rates of implant procedures, setting new standards in patient care.
Limitations
This review is limited by variability in study methodologies, including differences in sample sizes, follow-up durations, and evaluation metrics for biological space. Additionally, heterogeneity in measuring biological space dimensions, influenced by inconsistencies in imaging techniques and clinical protocols, poses a challenge in synthesizing results. The inclusion of different implant systems, restorative protocols, and patient populations further contributes to potential biases, making direct comparisons across studies difficult. Future research should prioritize standardized methodologies, such as uniform definitions of biological space and the adoption of advanced imaging technologies like CBCT, to ensure consistency. Furthermore, larger multicenter trials with diverse patient demographics and extended follow-up periods are essential to validate findings and enhance the generalizability of results.
CONCLUSION
The biological space is fundamental to the success of dental implants, providing a protective barrier and supporting peri-implant tissue health. Clinicians must prioritize its preservation through precise surgical placement, soft tissue management, and thoughtful prosthetic design. By respecting biological space, practitioners can achieve superior implant outcomes, enhancing both function and esthetics. The integration of modern imaging technologies and digital workflows holds promise for further improving biological space management and ensuring consistent clinical success.
ACKNOWLEDGMENTS
None.
CONFLICTS OF INTEREST
The authors declare that no conflict of interest.
REFERENCES
- Topçu AO, Yamalik N, Güncü GN, Tözüm TF, El H, Uysal S, et al. (2017). Implant-Site Related and Patient-Based Factors With the Potential to Impact Patients' Satisfaction, Quality of Life Measures and Perceptions Toward Dental Implant Treatment. Implant Dent. 26(4):581-591.
- Miri R, Shirzadeh A, Kermani H, Khajavi. (2017). Relationship and changes of primary and secondary stability in dental implants: a review. Int J Contemp Dent Med Rev. 2017:3011.
- Zhu G, Wang G, Li JJ. (2021). Advances in implant surface modifications to improve osseointegration. Mater Adv. 2(21):6901-6927.
- Hasegawa M, Saruta J, Hirota M, et al. (2020). A newly created meso-, micro-, and nano-scale rough titanium surface promotes bone-implant integration. Int J Mol Sci. 21:783.
- Wohrle PS. (2003). Nobel Perfect esthetic scalloped implant: Ratio nale for a new design. Clin Implant Dent Relat Res. 5(suppl 1):64-73.
- Noronha Oliveira M, Schunemann WVH, Mathew MT, Henriques B, Magini RS, Teughels W, et al. (2018). Can degradation products released from dental implants affect peri-implant tissues? J Periodontal Res. 53(1):1-11.
- Sahrmann P, Gilli F, Wiedemeier DB, Attin T, Schmidlin PR, Karygianni L. (2020). The Microbiome of Peri-Implantitis: A Systematic Review and Meta-Analysis. Microorganisms. 8(5):661.
- Sultan Z, Hafeji S, Tekin S, Habib S, Ullah R, Sefat F, et al. (2020). Titanium, zirconia, and polyetheretherketone (PEEK) as a dental implant material. Dental Implants. DOI:10.1016/b978-0-12-819586-4.00002-0.
- Marinescu ID, Rowe B, Ling Y, Wobker HG. (2015). Chapter 3—Abrasive Processes. In: Marinescu ID, Doi TK, Uhlmann E, editors. Handbook of Ceramics Grinding and Polishing. William Andrew Publishing; Boston, MA, USA. pp. 67-132.
- Londoño JJ, Ramos AM, Correa SA, Mesnard M. (2021). Review of expandable dental implants. Br J Oral Maxillofac Surg. 59(5):546-554.
- Gupta R, Gupta, N, Weber KK. Dental Implants. StatPearls 2021. Available at: https://europepmc.org/article/nbk/nbk470448
- Termeie DA. (2020). Periodontal Review Q & A. 2nd edn. Quintessence Publishing Co.; Batavia, IL, USA.
- Esposito M, Grusovin MG, Worthington HV. (2012). Interventions for replacing missing teeth: treatment of peri-implantitis. Cochrane Database Syst Rev. 1(1):CD004970.
- Tavelli L, Majzoub J, Kauffmann F, Rodriguez MV, Mancini L, Chan HL, et al. (2023). Coronally advanced flap versus tunnel technique for the treatment of peri-implant soft tissue dehiscences with the connective tissue graft: A randomized, controlled clinical trial. J Clin Periodontol. 50(7):980-995.
- Ajami E, Fu C, Wen HB, Bassett J, Park SJ, Pollard M. (2021). Early Bone Healing on Hydroxyapatite-Coated and Chemically-Modified Hydrophilic Implant Surfaces in an Ovine Model. Int J Mol Sci. 22(17):9361.
- Kim J, Adachi T. (2021). Cell-fate decision of mesenchymal stem cells toward osteocyte differentiation is committed by spheroid culture. Sci Rep. 11(1):13204.
- Sharma A, Waddell JN, Li KC, A Sharma L, Prior DJ, Duncan WJ. (2021). Is titanium-zirconium alloy a better alternative to pure titanium for oral implant? Composition, mechanical properties, and microstructure analysis. Saudi Dent J. 33(7):546-553.
 Abstract
Abstract  PDF
PDF