Past Issues
Ceramic Inlay Effectivness Versus other Restorative Treatments: A Literature Review
Aya A Salama1*, Omnia Nabil2, Mohamed A Mokhtar1, Mohamed M Radwan3
1Department of fixed prosthodontics, Faculty of Dentistry, MSA University, Egypt 2Department of fixed prosthodontics, Faculty of Dentistry, Cairo University, Egypt 3Department of fixed prosthodontics, Faculty of Dentistry, Beni Suef University, Egypt
*Corresponding Author: Aya Ahmed Salama, Lecturer in MSA University, Giza, Egypt 11567, 72 Bostan Street, Egypt.
Received: November 11, 2019 Published: December 18, 2019
ABSTRACT
Purpose: Long-term clinical studies is still required to give accurate outlook regarding the ceramic inlays, recent ceramic materials developments permitted the construction of more enhanced esthetic restorations as crowns and bridges, yet no conclusive studies yet regarding the effectiveness of ceramic inlays versus other posterior restorative materials.
Methods: A protocol of electronic and hand research was performed for English based researches in the MEDLINE database from 2000, till May 2019. Studies used in the current study were identified from in-vivo studies, in-vitro studies, previous systematic reviews, case reports.
Conclusion: Ceramic inlay retained restorations proved clinical significant success compared to the alternative other posterior restorative options available.
Keywords: Inlay; Ceramic; Gold restoration; composite inlay; Adhesive restoration
INTRODUCTION
Although ceramic materials have existed since the late century, the potentials for use in the posterior region have increased tremendously nowadays, this allowed ceramic restorations to replace many traditional restorations [1]. Dental ceramics started their applications in dentistry with denture teeth, and posterior crowns, yet, because of the inherent weakness in initial ceramic materials, they never came that popular. Recent ceramic materials developments permitted the construction of more enhanced esthetic restorations as crowns and bridges [2].
When more developments was introduced in the late 90's, significant improvements were noticed in the ceramic systems regarding their physical properties and strength and the most important enhancements of the adhesive properties, allowing further applications and indications for the dental ceramic restorations [3]. Before bonding of ceramic restorations, posterior teeth cavities were repaired using conventional amalgam and cast gold, but with today's high expectations and esthetic needs, patients will not accept a non-safe restoration or an expensive, and an unattractive restoration [4].
Clinicians are challenged everyday with restorative conditions demanding them to take judgmental choices about the correct selection of materials for improved function and aesthetics [3]. Patients are more pleased with treatment strategies that will offer ideal mastication but, still not lacking an esthetic perception, from this point, all ceramic restorations emerged [5].
METHODS
Search strategy
This literature review was conducted in view of the PICO elements. The PICOs (population, intervention, comparator, and outcome) question was defined as follows: Is the ceramic inlay efficacy compared to other posterior teeth restorative options?
Electronic databases search
A protocol of electronic and hand research was performed for English based researches in the MEDLINE database from 2000, till May 2019. Studies used in the current study were identified from in-vivo studies, in-vitro studies, previous systematic reviews, case reports.
RESULTS
Historical Outlook for dental ceramics
All-ceramic restorations were introduced to dentistry started with the Traditional feldspathic porcelain, it is industrialized from a powder and liquid. Feldspathic porcelain has increased its popularity in the 1960s [6]. It was cemented with conventional zinc phosphate cement. Even though it was highly appealing and very aesthetic restoration, it was unable to bond to enamel and dentin at the beginning, which led to many failures as fracture and de-bonding [7]. Few years later, aluminous porcelain was then introduced by McLean, it is characterized by the presence of scattered alumina particles that resists the crack development [8].
All-Ceramics material Development
The modern-day paradigm in restorative dentistry tends to be conservative in relation to removing healthy tooth structure unnecessarily [9], as the most common complication with metal-ceramic restorations is the need for over-reduction that might necessitate endodontic treatment [10]. Bonding makes it possible to save as much tooth structure as possible while satisfying the patients restorative desires and esthetic needs [11]. Added developments were produced the following two decades.
Dental Ceramic Systems
Starting the 80's dental ceramic materials available include:
Feldspathic (Glass) porcelain
It is the typical porcelain based ceramics, made of feldspar, kaolin, colorants and glass. Glass provides ceramics the enhanced translucent appearance. It is provided as powder and liquid or blocks that are being milled into desired restorations. It can match exactly enamel natural shades, can successfully mask less aesthetic restorations. [12]
Glass-infiltrated alumina
In-Ceram Alumina is an example of glass-infiltrated alumina, it is a material with sintered alumina glass-infiltrated substructure for anterior and posterior full coverage restorations as sufficient bonding will not be available [13]. Glass-infiltrated alumina has a flexural strength that range from 343 MPa up to 600 MPa depending on the type of dispersed particles. It is constructed with either slip-casting technique or computer-aided design/computer-aided manufacturing (CAD/CAM) [14].
Densely sintered aluminum oxide
Procera is the most famous example for this type of dental ceramic material. It is glass free, which gives it a very high flexural strength up to 650 MPa, with 99% pure aluminum oxide. It is better to be used in posterior region because of the high opacity of alumina particles, and the lack of translucency. No bonding is offered, so this limits its indication to full coverage restorations. It can be only fabricated using CAD/CAM technology [15].
Leucite-reinforced glass ceramics
Feldspathic porcelain generally has poor physical properties namely its low compressive strength of 70 MPa, this prompted the development of a reinforced generation of ceramics [16]. Two types of reinforcing particles were added to feldspathic porcelain for strengthening, leucite (1980’s) and lithium-disilicate (2000’s) [16]. IPS Empress from Ivoclar Vivadent, is an example of Lucite-reinforced glass ceramics. It depends on a leucite crystalline particles to strengthen its glass ceramic configurations. This ceramic material is considered a highly esthetic restorations. It is highly translucent, so tooth stump shade is very important because leucite-reinforced glass ceramics can't mask dark discolored tooth structure, or grey metallic implant abutments [17]. Its flexural strength is only 112 MPa. The highly esthetic ceramic restorations (crowns, inlays, onlays, vonlays, and veneers) are constructed either using pressing or CAD/CAM technology [18]. Lithium disilicate glass ceramics
IPS Empress II represents an example of lithium disilicate glass ceramics. It was developed primarily for three-unit bridges; they can be used to construct anterior/posterior crowns, partial coverage restorations. It has a flexural strength three times more than leucite reinforced material [19].
Yttrium tetragonal zirconia polycrystals
Incoris-TZI is an example of Yttrium tetragonal zirconia polycrystals (Y-TZP). Zirconia represent the highest strength, glass-free polycrystalline ceramic material used to construct anterior and posterior crown copings and fixed partial denture frameworks [20]. Flexural strength of the yttrium partially stabilized tetragonal zirconia is 900 MPa to 1,200 MPa. Esthetic feldspathic porcelain can be added over the zirconia coping using layering or pressing technique for better results [20].
Hybrid Ceramics Hybrid ceramics consist of esthetic silicate ceramics that are entirely interconnected evenly with a fine polymer setup. The polymer network offers the ceramic with some extent of elasticity comparable to that of dentin. Hybrid ceramics bonded using adhesive allows significantly greater and continuous stress tolerance than conventional non-adhesive ceramics [21].
Ceramic inlay parameters for success
Preparation criteria
Each type of ceramic material manufactures set the recommended inlay design features that matches the physical properties of the ceramic material, but in general, ceramic inlay preparation must have [22]:
- 8-10 degrees divergent axial walls in order to be able to seat the indirect ceramic inlay, and successfully scan the impression, no beveling should be done to prevent ceramic chipping.
- Round occluso-axial line angles.
- Rounded and smooth walls, and line angles to prevent stress accumulation and inlay fracture.
- 1.5-2 mm cavity depth depending on the strength of the restoration and the minimal thickness required.
- For most materials and systems, 1.5 mm width is sufficient
Ceramic inlay adhesive cementation
Ceramics are a brittle material that exhibits low tensile strength and usually low flexural strength. Being brittle material, requires it to be supported by a cement stress absorbing layer. Adhesive cementation act with the glass ceramics as a strong monoblock, with the proper resin cement adhesive system are a primary key in the success of inlay ceramic restorations. Either light or dual cured resin cements can be used, each has its pros and cons. Dual cured cements are of great use especially in inlay ceramics as the thickness of the inlay are usually more than 4 mm which doesn't allow full access to the light and polymerization of the resin [23], yet research has proven better long term success when light cured resin cements has been used for adhesive cementation of all-ceramic inlay restorations and this might be due to the risk of discoloration which is due to the rate of conversion of cured resin matrix [23]. Ceramic inlays transmit light better than composite resin inlays, this leads to greater degree of resin conversion [24].
Traditional cements like glass ionomer and zinc phosphate will make the ceramic inlay more reliable to fracture in comparison with the adhesive bonding of the inlays [25]. Resin modified glass ionomer was thought of as a substitute to conventional glass ionomer due to the higher strength and fluoride release, yet, it was debatable as fluoride release was for a short period of time, and strength is not high as adhesive resin [26]. Low viscosity resin cement will provide a durable micro-mechanical bond [26].
From a clinical point view, luting agent selection, and the ceramic surface treatment required depends on the type of ceramic material as indicated in (Table 1). Any glass based ceramics can be etched using hydrofluoric acid then silanated before cementation with adhesive resin cement, example to this feldspathic porcelain, lithium disilicate, and leucite-based glass ceramics. Adhesive resin cement provided enhanced bond strength with ceramic inlays [27]. Zirconium dioxide ZrO2 based ceramics, or densly sintered ALO, can't be etched, and therefore conventionally cemented with glass ionomer or ZnPo4 cements, phosphate resin modified cements can be used too [27].
Table 1: Different types of ceramic material, surface treatment needed, and the recommended luting agent.
|
Inlay ceramic material |
Recommended Ceramic treatment |
Required Coupling agent |
Recommended cement(s) |
|
Feldspathic porcelain |
Hydrofluoric acid etch |
Silane coupling agent |
Composite resin |
|
Leucite reinforced glass ceramics |
Hydrofluoric acid etch |
Silane coupling agent |
Composite resin |
|
Alumina reinforced glass ceramics |
Hydrofluoric acid etch |
Silane coupling agent |
Composite resin |
|
Lithium disilicate glass-ceramics |
Hydrofluoric acid etch |
Silane coupling agent |
Composite resin |
|
Dense sintered ZrO2 |
Metal/Zr primer |
NA |
Zinc phosphate, zinc poly-carboxylate, glass ionomer or phosphate modified resin cement |
|
Dense sintered AI2O3 |
NA |
NA |
Zinc phosphate, zinc poly-carboxylate, glass ionomer or phosphate modified resin cement |
|
Glass infiltrated zirconia |
NA |
NA |
Phosphate modified resin cement |
|
Glass infiltrated alumina |
NA |
NA |
Phosphate modified resin cement |
Finishing of ceramic inlay restoration
Sufficient finishing and polishing of the inlay restoration is very essential in order to prevent the abrasive effect of the rough ceramic restoration that will damage the enamel of the antagonist, and the risk of cracks development and chipping of the restorations [23].
Alternative restorations in posterior teeth
Three different classes were classified by Lutz et al [28], for the purpose of restoring posterior teeth, named as standards I, II, and III. Standard I describe the restoration that will maintain the tooth structure remaining, but has no function purposes, example to this is the temporary filling material. Standard II describes any restoration that will preserve the remaining tooth structure and will act as a functional substitute yet, it will not satisfy the patient aesthetic needs as desired, example to this amalgam restoration, and gold inlay retained restorations. Standard III describes a restoration that will restore the missing tooth structure, fulfil the functional requirement and with an enhanced esthetics, example to this class is the ceramic inlay retained restorations.
Metallic Amalgam Restorations
Amalgam posterior teeth restorative material has proved Amalgam restorations have proven to be a very tolerant, forgiving and durable restoration if the isolation issue is overcome which is unlike adhesive restorations. Amalgam is condensable material, which makes building up of marginal ridges and proximal contact more easily going, and this material literature history, clinical success, and survival is highly documented. Bonding of amalgam restorations has proven to decrease the microleakage significantly [29], which will reduce pulp inflammation, recurrent caries under the restoration, and definitely reduce post-operative sensitivity [30]. The disadvantages of amalgam restorations, is the unaesthetic appearance of the grayish metallic appearance, mercury release has become a world-wide health, and environmental issue that expresses a lot of concerns nowadays [31].
Cast gold inlay restorations
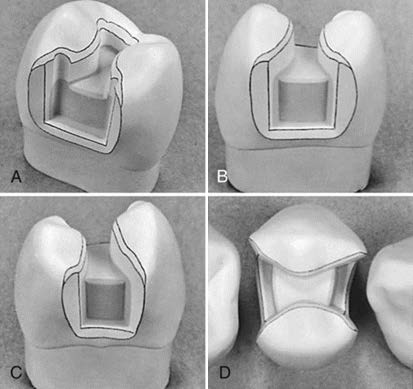
Cast-gold inlays are the standard level that every substitute posterior restoration should look to. Well fabricated gold inlays survival rates in literature is high, 70% survival in 15 years [32]. Gold inlays are reliable, strong restorations, indestructible in the oral fluids with no corrosive products as amalgam, dimensionally stable, insignificant wear on opponents, margins can be flared and beveled for better polishing and superior adaptability (Figure 1) and excellent production of tooth anatomy. They are the perfect restorations for large size high load restorations at the second molar, especially that it is nowadays considered an unaesthetic restoration. On the other hand, there were several studies that reported unsatisfactory results, which were mainly related to recurrent caries surrounding the gold restoration margins, loss of retention, yet, promising results can be seen later after introducing the adhesive cementation concept for posterior restorations [33].
Figure 1: Different views for gold-inlay tooth preparation.
Composite resin adhesive restorations
Recently, tooth- colored composite restorations combined with adhesive skills and knowledge, has increased tremendously as a posterior teeth restorative restoration [34]. Composite restorations tend to restore posterior teeth in a conservative approach that is not present or factor in most other alternative substitutes. They present excellent results when proximal ridges are still intact, as although they are less stiff than ceramics and have a modulus of elasticity close to dentin, they can still never restore or substitute the high load bearing proximal enamel ridges which is lost in large class II cavity restorations. The adhesively bonded restorations offer metal free, tooth structure colored substitutes, replicate the intact tooth before destruction in the terms of cusp protection, esthetics, and being reliable, and flexible restoration [35]. Composite adhesive restorations cannot depend on it when full cusp coverage is required, ceramic inlays and onlays are recommended in this step [35].
There is direct and in-direct composite technique of application, in most cases, direct adhesive composite is used for small to medium cavity size preparation. They only need one visit which is easier for both the patient and the clinician. Difficulties encountered with adhesive composite resin restorations is the marginal adaptation inaccuracies, material sensitive especially in the presence of oral fluids, placement difficulties, takes long time and effort to finish and polish a composite restoration, not easy to restore contacts and contours with direct composite increments, voids are hard to get rid-of which create a weak restoration, and post-operative sensitivity is unavoidable in many deep preparation cases [34].
As for the indirect adhesive composite restorations, they will offer great color match, save the time of the patients and the dentists, more feasibility to finish the restorations extra-orally. Yet, there is always high risk of marginal inaccuracies, extra laboratory time, which means extra cost, poor adhesion to the tooth compared to direct composite restorations, and material and technique sensitive [34].
The use of Ceramic inlays
Ceramic inlay indications
The indications of ceramic retained inlay restorations are the same as cast gold metal inlays restorations and added to it that it is a tooth colored requirement. They allow tooth conservatism and preserve the remaining tooth structure, Ceramic inlays can be conservative of tooth structure, and permit preservation of much coronal tissue. They are excellent aesthetic alternative to amalgam and gold inlay restorations and a stronger, durable restoration that can handle a large diameter cavity with loss of marginal ridge and wide diameter isthmus better than composite adhesive restorations. Posterior ceramic inlays will provide better physical properties, and higher flexural strength. The ceramic inlays drawbacks compared to direct technique composite restoration is the increased number of visits, greater cost due to the type of materials used, laboratory cooperation, and higher level of skill needed [36].
Ceramic inlay contraindications
Rosenstiel in his 4th edition book, stated that ceramic inlay retained restorations higher failure rates are anticipated when the patients are of poor oral hygiene and high caries index is observed. Faulty treatment plans also share its part in the ceramic failure causes, very high or excessive posterior load will not be taken well by the ceramic inlay, careful selection of indicated candidates should be performed. Excessive forces and stresses on the ceramic inlay even if high strength ceramics is used, will cause porcelain fracture, and failure of restoration. Full coverage crowns is indicated if para-functional habits is present, and use another substitute to ceramic inlay if there is a difficulty to achieve proper isolation and dry field, as this will affect the adhesive cementation procedure causing weakening of the ceramic inlay. The same goes for deep sub-gingival margins due to the difficulty in isolating the field [37].
Ceramic inlay as a fixed partial denture retainer
Long-term clinical studies is still required to give accurate outlook regarding the ceramic inlays as a retainer in a fixed partial denture. Some research studies, tested the retention of these partial coverage retainers and they were much less retentive than full coverage inlay retainers. Regarding their ability to tolerate high stresses and occlusal forces, ceramic materials as leucite-reinforced and lithium disilicate glass ceramics needed for adhesive bonding were not of sufficient high strength ceramics as zirconium oxide poly-crystalline ceramics which don't have the adhesive bonding capabilities [38]. It was suggested by some authors that veneering the fitting surface of zirconia ceramic inlay retainers with pressed lithium disilcate high silica content will give both advantages of high flexural strength and reliable adhesion with the resin luting agent [39].
Finite element analysis studies frequently tested stress distribution of multiple studies have analyzed stress distributions of ceramic inlay retained fixed partial dentures, higher stress concentration was found in the inlay retained design compared to full coverage retainer design by a 20% higher percentage [40,41]. Clinical studies with long-time follow-ups are necessary to evaluate and give accurate statistical results and conclusions of how ceramic inlay retainers with different ceramic materials will perform versus other retainer designs [42].
Ceramic inlay in literature
An aesthetic and durable restoration is what ceramic inlays offer, this is based on its ability to replicate anatomic contours, good marginal adaptation, strengthen the residual tooth structure through bonding to the tooth [43].
Large size and deep restoration showed better survival rates with all-ceramic inlays compared to its posterior teeth alternative substitutes as amalgam, adhesive composite, and gold inlays. This is probably due to the high flexural strength presented by the ceramic material. Different types of all ceramic materials is available in the market, each has its own advantage and disadvantage as stated earlier in this review [44].
Ceramic inlays cavity preparation criteria plays a fundamental factor in the success of the restoration, all line and point angles should be rounded, no sharp preparations to avoid excessive stress concentration that will fracture the ceramic restoration. Flat and smooth gingival and floor seat of the preparation is mandatory for long survival of the restoration. 90 degrees cavo surface angle, with divergent walls and blocked undercuts in order to save as tooth structure as much as possible (44). Ryge and Cvar [45] proposed an assessment criteria for dental restorations, which was of great reliability for the past years and still is (Table 2).
Table 2: Clinical assessment criteria for inlays, using Modified (USPHS) United States Public Health Service criteria.
|
Marginal accuracy |
|
|
A |
Margin not visible and marked, no catch with probe, discoloration of the margins is not present. |
|
B |
There is a margin catch with probe, yet, no gap nor is chipping felt. Enamel uncovered but polished, and minimal marginal discoloration is seen. |
|
C |
Chipping and marginal gap is felt with probe, uncovered dentin, non-polished surface is present, obvious discoloration is noted with secondary caries and unaccepted restoration. |
|
D |
Incomplete fracture, full restoration fracture, loose restoration, abutment tooth fracture. |
|
Anatomic contour |
|
|
A |
Right contour with closely fitting proximal contacts, and checked with waxed dental floss. Wear facets are not present on the restoration nor the antagonist. |
|
B |
Minimal under or over contoured restoration, limited wear facets less than 2mm on the restoration and antagonist teeth. Slightly open proximal contact. |
|
C |
Severe under or over contoured restoration, large wear facets less more than 2mm on the restoration and antagonist teeth. Absence of proximal contact. |
|
Surface quality |
|
|
A |
Shiny, Smooth, and polished restoration. |
|
B |
Minimal roughness and dull restoration. |
|
C |
Rough, irregular, full of pits and pores. Unacceptable and can't be finished. |
Another clinical assessment method was applied by a study examining IPS‐Empress [46]. A criteria of (A) was specified if no corrections was required for the restoration, and no changes clinically was observed. A criteria of (B) was specified if minor corrections was required for the restoration, no threatening to remaining tooth structure nor pulp and periodontal ligament. Secondary caries is not present, and no loss of periodontal attachment. Class (B) is considered acceptable and no repair is needed. A criteria of (C & D) was given if major corrections was required for the restoration, threatening to remaining tooth structure, pulp and periodontal ligament was found. Secondary caries is present with loss of periodontal attachment. Total repair of the restoration is needed with class (C& D) as it is unacceptable restoration (Table 3).
Failure reasons were further classified into technical like fracture, loss of retention, and wear facets of the restoration and biological causes like tooth fracture, recurrent caries, and extraction of the tooth.
Table 3: The findings of Ceramic inlay restorations based upon classification of outcome and the clinical re‐evaluation at the time of follow-up.
|
Rating |
Restoration description |
Outcome |
Re-evaluation time |
|---|---|---|---|
|
A |
No adjustment needed |
Success |
Follow-up date |
|
B |
Minimal shortcoming without compromising of tooth structure, pulp, or periodontal apparatus. |
Success |
Follow-up date |
|
C, D |
Threaten of tooth structure, pulp, and periodontal apparatus. Replacement or repair is mandatory. |
Failure |
Follow-up date |
A clinical study evaluated ceramic inlays performance, and concluded that no secondary caries was found around the margins, and the only drawback was discoloration of the margins, and that they are an excellent reliable tool for the restoration of posterior teeth [47]. Another research was performed and stated that the survival rate of ceramic inlays was 100% versus its comparator the adhesive composite restoration that also recorded a good survival rate of 90% [48]. This was followed by a systematic review study evaluating the quality of ceramic inlay restorations for reconstruction of posterior teeth compared to other alternatives. The authors concluded that no significant differences was found between ceramic material and all other substitute restorative options for a follow-up period up to 1 year, stating that long-term clinical studies are still needed for conclusive long-term results [1].
A 10 years follow-up study evaluated the performance of ceramic inlays class II defect, and concluded that the clinical survival was significant and patients acceptance were high [49]. Leucite-reinforced glass ceramics was assessed for its performance and showed a very high clinical survival rates in very large size cavities that can't be restored with adhesive composite resin [50].
Another study testing the clinical efficiency of adhesive composite inlays and found that it proved high success rate and it is not influenced by the size of the tooth defect, and that bonded restorations strengthen the residual tooth structure and should be indicated for any posterior tooth defect [51]. Lange in his clinical research found that ceramic inlays indirectly fabricated showed superior marginal accuracy, color stability and match, and better anatomic contour than direct bonded composite restorations [52].
A systematic review article was published in 2018, questioning the longevity of ceramic inlays restorations, and the following were concluded: Exact shade and color stability will be achieved using the proper ceramic material that matches the translucency of the tooth to be restored, that in most cases no demarcation is felt between the tooth and the restoration. Higher physical properties compared to direct composite restorations, enamel margins provide strong adhesive bond with the resin cement and tooth structure, reducing micro-leakage compared to Conventional amalgam and gold inlay restorations. Margins on dentin still expressed micro-leakage even with advanced adhesive bonding systems [33]
After the introduction of strong adhesive composite restorations into the market, ceramic inlays became less accepted and all clinicians thought from an economic point of view, about the cost difference between ceramic material and composite resins. Yet, after long clinical observations, the question popped out again, whether composite resin are durable enough to avoid discoloration, marginal leakage, wear, and high survival rate [52].
Nowadays, posterior ceramic inlays material selections comprise the use of a high strength ceramic material, or using a high-strength ceramic sub-structure material that will be veneered with a more translucent adhesive more appealing veneer. The second method has vanished in the past years, but it started to reintroduce again, after the increase use of zirconia as a superior strength material. Improved combination of aesthetics, strength, and adhesive bonding qualities are the main focus of manufactures lately.
CONCLUSION
Ceramic inlay retained restorations proved clinical significant success compared to the alternative other posterior restorative options available.
Conflict of interest
The authors declare no conflict of interests.
Author Contribution
Aya Salama: Project development, Data Collection, Manuscript writing.
Omnia Nabil: Data Collection, Manuscript writing.
Mohamed A Mokhtar: Data analysis, Manuscript revising.
Mohamed M Radwan: Manuscript revising, Final approval.
REFERENCES:
- Hayashi M, Wilson NH, Yeung CA (2003). Systematic review of ceramic inlays. Clin Oral Investig 7(1):8-19.
- Kelly JR, Nishimura I, Campbell SD (1996) Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent Jan 75(1): 18-32.
- Raigrodski AJ (2004) Contemporary materials and technologies for all-ceramic fixed partial dentures: a review of the literature. J Prosthet Dent 92: 557–562.
- Friedl KH, Hiller KA, Schmalz G (1997) Clinical and quantitative marginal analysis of feldspathic ceramic inlays at 4 years. Clin Oral Investig 1 (4): 163-8.
- Santos MJ, Costa MD, Rubo JH, Pegoraro LF, Santos GC Jr (2015) Current all-ceramic systems in dentistry: a review. Compend Contin Educ Dent 36: 31–37.
- McLaren EA (1998) All-ceramic alternatives to conventional metal-ceramic restorations. Compend Contin Educ Dent 19: 307-312.
- Mackert JR (1992) Side-effects of dental ceramics. Adv Dent Res 6: 90–3.
- McLean JW, Hughes TH (1965) The reinforcement of dental porcelain with ceramic oxides. Br Dent J 119: 251-267.
- McLaren EA, Whiteman YY (2010). Ceramics: rationale for material selection. Compend Contin Educ Dent 31: 666–668.
- Goodacre CJ, Bernal G, Rungcharassaeng K (2003) Clinical complications in fixed prosthodontics. J Prosthet Dent 90: 31–41.
- Strassler HE (2007) Minimally invasive porcelain veneers: indications for a conservative esthetic dentistry treatment modality). Gen Dent 55(7): 686-694.
- Sadowsky SJ (2006) An overview of treatment considerations for esthetic restorations: a review of the literature. J Prosthet Dent 96(6): 433-442.
- Seghi RR, Sorensen JA (1995) Relative flexural strength of six new ceramic materials. Int J Prosthodont 8: 239-246.
- Bindl A, Mormann WH (2002) An up to 5-year clinical evaluation of posterior In-Ceram CAD/CAM core crowns. Int J Prosthodont 15: 451–456.
- Fradeani M, D'Amelio M, Redemagni M (2005) Five-year follow-up with Procera all-ceramic crowns. Quintessence Int 36: 105–113.
- Anusavice K, Shen C, Rawls R (2013). Phillips’ Science of Dental Material.12th ed. St. Louis MI: Saunders, Elsevier Inc., 418–473.
- Ivoclar/Vivadent (2014) The results of twelve years of research. IPS e.max Scientific Report Vol. 2. [Internet]
- Sjogren G, Lantto R, Granberg ASundström BO, Tillberg A (1999). Clinical examination of leucite-reinforced glass-ceramic crowns (Empress) in general practice: a retrospective study Int J Prosthodont 12: 122–128.
- Pieger S, Salman A, Bidra AS (2014) Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent 112: 22–30.
- Raigrodski AJ, Hillstead MB, Meng GK Chung KH (2012) Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent 107: 170–177.
- Kassardjian V, Varma S, Andiappan M Creugers NH Bartlett D (2016) A systematic review and meta-analysis of the longevity of anterior and posterior all-ceramic crowns. J Dent 55: 1-6.
- Frankenberger R, Reinelt C, Petschelt A, Krämer N (2009) Operator vs material influence on clinical outcome of bonded ceramic inlays. Dent Mater 25(8): 960-968.
- Schwass DR, Lyons KM, Purten DG (2013) How long will it last? The expected longevity of prosthodontic and restorative treatment. N Z Dent J 109(3): 98-105.
- Shimura R, Nikaido T, Yamauti M (2005) Influence of curing method and storage condition on micro-hardness of dual-cure resin cements. Dent Mater J 24(1): 70–75.
- Filho AM, Vieira LCC, Araujo E, Baratieri LN (2003) Ceramic inlays and onlays: clinical procedures for predictable results. J Esthet Restor Dent 15(6): 338–351.
- Van Dijken JWV, Örmin A, Olofsson AL (1999) Clinical performance of pressed inlays luted with resin-modified glass ionomer and autopolymerizing resin composite cements. J Prosthet Dent 82(5): 529–535.
- Pallesen U, van Dijken JWV (2000) An 8-year evaluation of sintered ceramic and glass ceramic inlays processed by the CEREC CAD/CAM system. Eur J Oral Sci 108(3): 239–246.
- Lutz F, Krejci I, Besek, M (1997). The missing standards. PPAD 9(5): 541-548.
- Neme AL, Evans DB, Maxson BB (2000) Evaluation of dental adhesive systems with amalgam and resin composite restorations: comparison of microleakage and bond strength results. Oper Dent 25(6): 512–519.
- Bonsor SJ (2011) Bonded amalgams and their use in clinical practice. Dent Update 38(4): 222–230.
- Shraim A, Alsuhaimi A, Al-Thakafy JT (2011) Dental clinics: a point pollution source, not only of mercury but also of other amalgam constituents. Chemosphere 84(8): 1133–1139.
- Studer S P, Wettstein F, Lehner, C, Zullo TG, Schärer P (2000) Long‐term survival estimates of cast gold inlays and onlays with their analysis of failures. J Oral Rehabil 27(6): 461-472.
- Abduo J, Sambrook RJ (2018) Longevity of ceramic onlays: A systematic review. J Esthet Restor Dent 30(3): 193-215.
- Magne P, Belser U (2002) Bonded Porcelain Restorations in the Anterior Dentition - A Biomimetic Approach. Quintessence Publishing Co, Inc., Berlin, Germany.
- Dietschi D, Spreafico R (1997) Adhesive Metal Free Restorations. Quintessence Publishing Co, Inc., Berlin, Germany.
- Cramer NB, Stansbury JW, Bowman CN (2011) Recent advances and developments in composite dental restorative materials. J Dent Res 90(4): 402-416.
- Rosenstiel SF, Land MF, Fujimoto J (2006) Contemporary Fixed Prosthodontics [4th Ed.], Elsevier, St Louis, USA, 327.
- Ohlmann B, Rammelsberg P, Schmitter M, Schwarz S, Gabbert O (2008) All-ceramic inlay-retained fixed partial dentures: preliminary results from a clinical study. J Dent 36 (9): 692–696.
- Monaco C, Cardelli P, Bolognesi M, Scotti R, Ozcan M (2012) Inlay-retained zirconia fixed dental prosthesis: clinical and laboratory procedures. Eur J Esthet Dent 7(1): 48–60.
- Thompson MC, Field CJ, Swain MV (2011) The all-ceramic, inlay supported fixed partial denture. Part 2. Fixed partial denture design: a finite element analysis. Aust Dent J 56(3): 302–311.
- Thompson MC, Field CJ, Swain MV (2012) The all-ceramic, inlay supported fixed partial denture. Part 3. Experimental approach for validating the finite element analysis. Aust Dent J 57(1):23–30.
- Wolfart S, Kern M (2006) A new design for all-ceramic inlay-retained fixed partial dentures: a report of 2 cases. Quintessence Int 37(1): 27–33.
- Fradeani M, Aquilano A, Bassein L (1997) Longitudinal study of pressed glass-ceramic inlays for four and a half years. J Prosthet Dent 78: 346–353.
- Priti D Desai, Pathik P Patel, Khyati Shah, Pankaj N Patel (2014) All Ceramic Inlay: A Case Report. J Res Adv Dent 3(2s): 72-77.
- Ryge G & Cvar J (1975) Criteria for the Clinical Evaluation of Dental Restorative Materials and Techniques. US Public Health Service Publication No. 790‐244.
- Studer S, Lehner C, Brodbeck U, Schärer P (1996) Short‐term results of IPS‐Empress inlays and onlays. J Prosthodont 5(4): 277-287.
- Fuzzi M, Rappelli G (1991) Ceramic inlays: clinical assessment and survival rate. J Adhes Dent 1(1): 71-79.
- Manhart J, Scheibenbogen-Fuchsbrunner A, Chen HY, Hickel R (2000) A 2-year clinical study of composite and ceramic inlays. Clin Oral Investig 4(4): 192-198.
- Sjögren G, Molin M, van Dijken JW (2004) A 10-year prospective evaluation of CAD/CAM-manufactured (Cerec) ceramic inlays cemented with a chemically cured or dual-cured resin composite. Int J Prosthodont 17(2): 241-246.
- Krämer N, Frankenberger R (2005) Clinical performance of bonded leucite-reinforced glass ceramic inlays and onlays after eight years. Dent Mater 21(3): 262–271.
- Barone A, Derchi G, Rossi A, Marconcini S, Covani U (2008) Longitudinal clinical evaluation of bonded composite inlays: a 3-year study. Quintessence Int 39(1): 65-71.
- RT Lange, P Pfeiffer (2009) Clinical Evaluation of Ceramic Inlays Compared to Composite Restorations. Oper Dent 34(3): 263-272
Copyright: Salama AA, et al. © 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Salama AA (2019). Ceramic Inlay Effectivness Versus other Restorative Treatments: A Literature Review. Dental 1(1): 3.
 Abstract
Abstract  PDF
PDF