Past Issues
Awareness and Preference of General Dental Practitioners towards Pre-Prosthetic Surgery as an Adjunctive to Complete Denture Therapy
Maraai Orafi1, Gazia Mohamed EL Bakoush2
1Maraai Orafi, Assistant professor and consultant, Department of oral and maxillofacial surgery, University of Benghazi, Benghazi, Libya
2Gazia Mohamed EL Bakoush, Assistant lecturer, Department of prosthodotics, University of Benghazi, Benghazi, Libya
*Corresponding Author
Maraai Orafi, Assistant professor and consultant, Department of oral and maxillofacial surgery, University of Benghazi, Benghazi, Libya, Tel: 00218915106775; 00218925106775; E-mail: [email protected]
Received Date: April 29, 2021
Publication Date: July 23, 2021
ABSTRACT
Objective: The aim of this study is to evaluate the attitude and awareness of sample of Libyan dentists towards preprosthetic surgery.
Materials and method: An observational study was undertaken for 150 registered dentists with a Bachelor of Dental Surgery degree, currently practicing in different cities of Libya. Only 109 dentists respond to our questions. Dentists with less than 5 years in Practice and who have no experience with removable prosthesis were excluded. This study was approved by the research ethical committee of Faculty of Dentistry-Benghazi University. Previous studies were used to prepare a questionnaire which includes questions about personal data, awareness and preference of dentist of preprosthetic surgery. Questionnaire was assessed by two expert oral- maxillofacial surgeon and prosthodontist.
Results: Out of 150 dentists to whom the questionnaire was sent, only 109 answered the questions. The study included 64 (58.7%) male and 45 (41.3%) female with male to female ratio 1.4:1. The age range of the participant was 30 to 52 years old. Regarding the years of practice, 18.1% had 5 years, 26.7% had 5-10 years and majority (55.2%) had more than 10 years of experience in practice of removable prosthesis. 41.9 % of participant constructing more than 10 dentures per year, 22.9% of dentists perform 5-10 denture insertion per year and 35.2% perform 3-5 dentures per year.
Conclusion: For surgeons to satisfy the needs of denture providers, it is advisable that oral and maxillofacial surgeons consult with the dentists who will construct the prosthesis rather than relying solely on their own opinion about what should be done for the patient.
KEYWORDS: Implant; Graft; Preprosthetic; Surgery
INTRODUCTION
The evolutionary cycle has selected a masticatory system, which is functionally efficient using natural teeth and an omnivorous diet [1]. This system would be designed in totally different fashion due to the loss of natural teeth after extraction [1] and bone resorption [2,3]. The results of this resorption are accelerated by wearing dentures and tend to affect the mandible more severely than the maxilla [2,4]. Dentures are rigid pieces of acrylic resin which are shaped to fit the soft tissue covering of the jaws and be compatible with the functioning and ever changing oral environment [1]. No denture, regardless of how well it is constructed, can overcome the limitations of the foundation on which it is placed [1,4]. In practice we encounter many patients for whom an ideal treatment from prosthodontics point of view is not possible without resorting to preconditioning of oral tissues by means of surgical procedures [1,2,4]. These procedures constitute the pre-prosthetic surgical preparation [1,2,4,5].
Pre-prosthetic surgery is an integral part of complete denture prosthodontics [5]. The ultimate goal of pre-prosthetic surgery is to prepare a mouth to receive a dental prosthesis by redesigning and smoothing bony edges which would otherwise cause hindrance in restoration of optimum health and function [5].
Preprosthetic surgery involves operations aiming to eliminate certain lesions or abnormalities of the hard and soft tissues of the jaws so that the subsequent placement of the prosthetic appliance is successful [1,2,4,5]. It is therefore important for oral and maxillofacial surgeon and the prosthodontist to be acutely aware of the problems faced by the other and to understand what can be done in a joint effort to resolve these problems [3]. The aim of this study is to evaluate the attitude and awareness of sample of Libyan dentists towards preprosthetic surgery.
MATERIAL AND METHODS
An observational study was undertaken for 150 registered dentists with a Bachelor of Dental Surgery degree, currently practicing in different cities of Libya. Only 109 dentists respond to our questions. Dentists with <5 years in Practice and who have no experience with removable prosthesis were excluded. This study was approved by the research ethical committee of Faculty of Dentistry-Benghazi University. Previous studies were used to prepare a questionnaire which includes questions about personal data, awareness and preference of dentist of preprosthetic surgery. Questionnaire was assessed by two expert oral- maxillofacial surgeon and prosthodontist (appendix 1).
Using Google form software [6] questionnaire was distributed electronically to 150 general dentists fulfilling the inclusion criteria to be a part of this study. Essentially, the questions dealt awareness of dentists toward types of surgical techniques that required helping success of dentures. Second group of question concerned about preferred method of augmentation, critical areas of vestibular depth, favoured tissue for vestibular grafting, minimal requirements for alveolar height, and opinions about loss of vestibular depth after different soft tissue grafting procedures. Data collected and analysed using Google form software.
RESULTS
Out of 150 dentists to whom the questionnaire was sent, only 109 answered the questions. The study included 64 (58.7%) male and 45 (41.3%) female with male to female ratio 1.4:1. The age range of the participant was 30 to 52 years old. Regarding the years of practice, 18.1% had 5 years, 26.7% had 5-10 years and majority (55.2%) had more than 10 years of experience in practice of removable prosthesis. 41.9% of participant constructing more than 10 dentures per year, 22.9% of dentists perform 5-10 denture insertion per year and 35.2% perform 3-5 dentures per year.
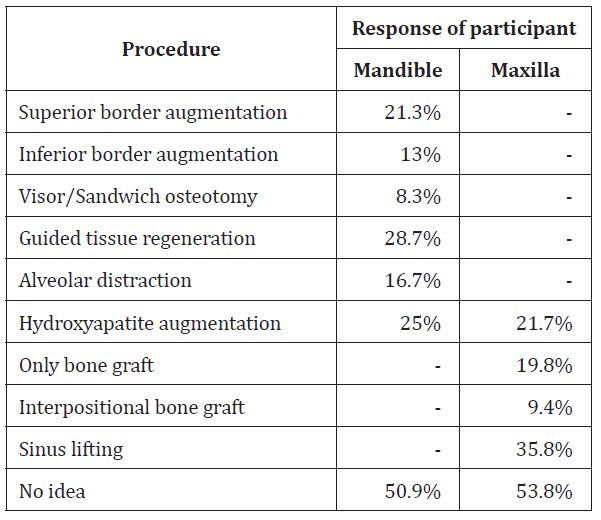
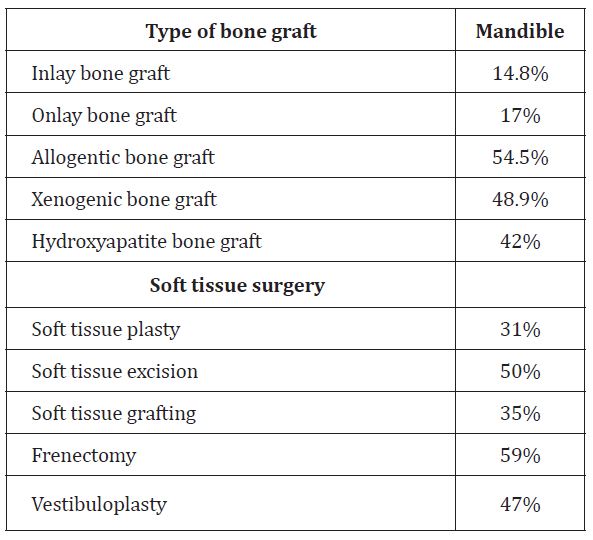
Answers to questions of awareness of ridge augmentation procedures revealed that 50.9% and 53.8 % of participants they have no idea about the mandibular and maxillary surgeries respectively. Table 1 shows response to these questions. Allogenic bone graft (54.5%) was the most familiar method among the participant whereas frenectomy (59%) was the most selected answer among the soft tissue surgeries. Table 2 show the responses to types of bone graft and soft tissue surgeries. About 88% of our sample they have not known what is the percentage of vestibular loss that they have seen in the first year after a mandibular vestibuloplasty with a mucosal or a skin graft?
Table 1: Answers to question are you familiar with the following ridge augmentation procedure?
Table 2: Responses to types of bone graft and soft tissue surgeries.
With respect to preference, most of responders (65%) keep the choice of type of bone graft for the surgeon, while 16% and 18% prefer allogenic and xenograft respectively. The most referred soft tissue surgery was vestibuloplasty (61.5%) whereas the least was soft tissues plasty (21.9%).
The area the mandibular vestibule that perceived as the most critical in obtaining maximal depth if vestibuloplasty to be performed was buccal shelf area in opinion of 51.9% of dentists followed by mentalis region (41.9%), mylohyoid area (25.8%), and genioglossal area (9.7%). The palatal mucosa (44.6%) was the most selected tissue type for vestibuloplasty with graft whereas 33.7% of dentists had no preference in type of tissues. The responses to question what is minimum mandibular bone height that perceived as necessary for denture construction? were 16.2% for 4-5mm, 32.4% for 6-10 mm, 10.5% for 10-20mm and 41% they don’t know. 80 of dentists in this study evaluate the hard tissue status before denture construction and 56.9% consult the oral and maxillofacial surgeon (OMFS) about soft and hard tissue defects and 6.4 % they don’t consult OMFS, 49.4% of them refer the patient for expert while 32.5% did some surgical procedures rather than referring patients.
Majority (53.7%) of dentist’s advice dental implants to reconstruct patient’s complete dentures. 28.4% of them put dental implants by themselves while 45% refer the patient for surgeon for implant insertion. Most of participant (45.7%-48.1%) had no experience with method of atrophic ridge augmentation and 29.2%-34.3% prefer dental implant to overcome this problem.
DISCUSSION
Majority of participant (55.2%) of this study had more than 10 years in practice of removable prosthodontics, and most of them (41.9%) construct more than 10 dentures per year. Several clinicians and patients believe that the success of dental treatment is affected by the experience of dentists. Prosthodontics experience of a clinician affected the satisfaction ratings of a complete denture wearer [7].
It is not a surprise to find approximately half of dentists questioned have not experience nor idea about ridge augmentation procedures in both atrophic mandible and maxilla as removable prosthesis are annoying to patients and dentists are usually concerned more about implant dentistry than unpredictable results of dentures and also rapid progress of dental implants attract dentists to solve problems of retention, stability and comfort of conventional dentures [8]. Even with prosthodontists still 6% had no preference and 9% lacked experience with ridge augmentation procedures [3].
29.2% and 34.3%of respondents of this study prefer dental implant as a method of augmentation of atrophic ridge of maxilla and mandible respectively. In a previous study [3] 10 to 29% of prosthodontists chose implants to deal with atrophic ridges. The preference of dental implants among dentists and prosthodontist may justify by high implant success [9] and patient’s satisfactions [10] toward implant retained prosthesis.
May because of new advances in guided tissue regeneration and sinus lift procedures [11], 28.7 and 35.8% of our participants respectively aware of these procedures. 21.7 to 25% was the percentage of awareness for hydroxyapatite augmentation, which is well known for bone regeneration for filling of defects from ancient times. Emerging technology has made the dreams of clinicians to realize the use of hydroxyapatite in different forms for various purposes both in vivo and vitro [12].
Our finding revealed that recognition of techniques that mostly performed under general anaesthesia and required special settings such as superior (21.3%) and inferior (13%) border augmentation, osteotomies (8.3%), onlay (19.8%) and interpositional (9.4%) bone grafts, and alveolar distraction (16.7%) was lower than other procedures practicizedin dental office under local anaesthesia.
Hence the surgeon’s role is to produce an environment in which esthetics and function may be optimized by manipulating, augmenting, or replacing soft and/or hard tissues [13], our responders may accordingly kept the choice of type of bone graft for the surgeon despite they were familiar with all types of bone grafts with high percentage of recognition for allogenic (54.5%) and xenogenic (48.9%) types.
It was mentioned that, the most commonly performed soft tissue procedure is frenectomy [14] and this is consistent with our results where frenectomy (59%), soft tissue excision (50%), and vestibuloplasty (47%) were most familiar among our group. These techniques along with soft tissues grafts were referred in a higher manner than other surgeries.
If vestibuloplasty and graft are to be performed on a patient, the tissue type preferred mostly by participant was palatal mucosa (44.6%), followed by buccal mucosa (19.8%) and skin (7.9%) and 33.7% of participants had no preference. From these infers that there is no clearly superior type. Mucosa is very resilient, provides a good colour match, and is easily obtainable from a nondistant secondary surgical site. However, it is limited in quantity and* has a tendency to ulcerate under pressure [3]. Moreover, when taken from the palate it can produce a painful donor site, and when taken from the cheek it can result in a contracted scar [3]. Skin, by contrast, is obtainable in much greater quantities, usually reacts to pressure by hyperkeratosis rather than ulceration, and is generally less painful under load [3]. However, it is less resilient, it requires a distant secondary surgical site, it has diminished touch perception, and, if cut too thick, it may result in growth of hair [3]. Since both skin and mucosa have major advantages as well as disadvantages, the prosthodontic considerations may be more important than the surgical considerations in making the final choice. There appears to be a need for greatercollaboration between the prosthodontist and the oral and maxillofacial surgeon in establishing specific indications for use of skin and oral mucosal grafts [3].
Buccal shelf area and mentalis region were perceived as the most critical in obtaining maximal depth in cases of vestibuloplasty. This is consistent with previous reports [15] and indicates high level of awareness of present study participants regarding this context.
CONCLUSION
It is clear from this survey that there is no consensus in many areas related to the surgical management of the prosthodontic patient, including adequate ridge height and the critical regions for attaining maximum vestibular depth. For surgeons to satisfy the needs of denture providers, it is advisable that oral and maxillofacial surgeons consult with the dentists who will construct the prosthesis rather than relying solely on their own opinion about what should be done for the patient.
LIMITATION OF THE STUDY
To determine the actual awareness of dental practitioner/specialists, a representative and randomized sample is required. However, the primary aim of this study was to evaluate the attitude and awareness of a selected sample of Libyan dentists. Questionnaire is a well-established strategy for data collection. However, it has its own limitations. For example, social desirability bias and non-response rate which may affect the representativeness of the sample and the quality of the information [16]. However, no personal information was sought and the participation was voluntary. So these biases would be of less impact in the current study. In addition the response rate in the current study was relatively high (72%).
FUNDING INFORMATION
No funding was obtained.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
ETHICAL APPROVAL
The study was in accordance with the ethical standards of the institutional research committee of Benghazi University and approval was OBTAINED.
INFORMED CONSENT
Using the Google form software freely enables the responders to agree or refuse answering the questionnaire. In top of the questionnaire, an explanation of aim of the study and statement of agreement to participate were written.
REFERENCES
- Tanu G, Jay V, Jagdeesh HG, Ashish C, Anurag H. (2009). Preprosthetic surgery. Heal Talk.
- Haripriya C, Khadar VS. (2016). Preprosthetic Surgery: Review of Literature.
- Larry RM, David A, Daniel ML. Prosthodontists’ preference in preprosthetic Surgery.
- Sahil Choudhari V, Rakshagan, Ashish RJ. (2018). Evolution in preprosthetic surgery current trends: A Review.
- Medha Vivek Bhuskute, Lt. Col Ravi GK Shet. Preprosthetic Surgery: An Adjunct to complete Denture Therpy. Journal of the international clinicle dental research organization. January 2019.
- Google forms: https://docs.google.com/forms?usp=mkt_forms.
- Kimoto S, Kimoto K, Kitamura A, Saita M, Iijima M, et al. (2013). Effect of dentist’s clinical experience on satisfaction of a complete denture. Journal of oral rehabilitation. 40:940-947.
- Misch CE. (2001). The importance of dental implants. Gen Dent. 49(1):38-45.
- Simomis P, Dufour T, Tenenbaum H. (2010). Long-term implant survival and success: a 10-16-years follow-up of non-submerged dental implants. Clin Oral Implants Res. 21(7):772-7.
- Susanne A, Anna RV, Annalisa P, Gerardo La M, Stefano Di C, et al. (2010). Patient satisfication with oral implant rehabilitation: evaluation of responses to a questionnaire. Annali di stomatologia. 1(3-4):2-8.
- Yazad G. (2017). Sinus Grafts: Science and Techniques-Then and Now. J Maxillofac Oral Surg. 16(2):135-144.
- Vivekanand SK, Suydheer K, Krishna PL. (2016). Hydroxyapatite-past, present and future in bone regeneration. Bone and tissue regeneration insighs.
- Hillel E, Robert K, Anthony S. (2015). Preprosthetic surgery. Oral Maxillofacial Surg Clin N Am. 459–472.
- Nurul, Syamimi, Binti Mohd Azlan, Sunil, SantohoshKumar MP, Revathi D. (2020). Analysis of preprosthetic surgeries performed in a privatedental institution. Int J Res Pharm Sci. 11(SPL3):1737-1742.
- Christian MS, Tobias M, Rainer L, Falk W, Friedrich W. Neukam and Karl Andreas Schlegel. Long-term outcomes after vestibuloplasty with a porcine collagen membrane (Mucograft) versus the free gingival graft: a comparative prospective clinical trial.
- Edwards PJ, Roberts I, Clarke MJ. (2009). Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 3:MR000008.
Appendix 1: Questionnaire to study Awareness and Preference of general dental practitioners towards pre-prosthetic surgery as an adjunctive to complete denture therapy
Aim: Is to evaluate the attitude and awareness of sample of Libyan dentists towards preprosthetic surgery.
Dear dentist/dental specialist: Please if you agree to participate in this study, answer the questions below.
General data: Age ……………………. Gender ……………… Qualifications ……………………………...
1. Are you
- Consultant in prosthodontics
- Specialist in prosthodontics
- General Practioner in dentistry
2. How many years you are practicing?
- 5 years
- 5-10 years
- More than 10 years
3. How many cases do you construct complete denature per a year?
- 3-5
- 5-10
- More than 10 dentures.
Awareness:
4. Are you familiar with the following mandibular ridge augmentation procedures?
- Superior border augmentation
- Inferior border augmentation
- Hydroxyapatite augmentation
- Guided bone regeneration
- Visor osteotomy, sandwich osteotomy, or combination
- Alveolar distraction
- No idea
5. Are you familiar with the following maxillary ridge augmentation procedures?
- Onlay bone graft
- Sinus lift procedures
- interpositional bone grafts
- Max. Hydroxyapatite augmentation
- No idea
6. Are you familiar with types of bone graft?
- Inlay bone graft
- Onlay bone graft
- Allogenic bone graft
- Xenograft bone graft
- Hydroxyapatite bone graft.
7. Are you familiar with following soft tissues surgery?
- Soft tissues plasty
- Soft tissues excision
- Soft tissues grafting
- Frenectomy and muscular attachment
- Vestibuloplasty.
8. Do you know the percentage of vestibular loss that you have seen in the first year after a mandibular vestibuloplasty with a skin graft? Yes ( ) No ( ).
9. Do you know, what is the percentage of vestibular loss that you have seen in the first year after a mandibular vestibuloplasty with a mucosal graft? Yes ( ) No ( ).
Preference:
10. What types of bone graft you preferred to your patient
- Inlay bone graft
- Onlay bone graft
- Allogenic bone graft
- Xenograft bone graft
- Hydroxyapatite bone graft
- You keep this choice for the surgeon
11. Do you refer cases with following soft tissues defect for surgery?
- Soft tissues plasty
- Soft tissues excision
- Soft tissues grafting
- Frenectomy and muscular attachment
- Vestibuloplasty
12. What is the minimum mandibular bone height that you perceive as necessary for construction of denture?
- 4- 5 mm
- 6- 10 mm
- 10- 20 mm
- I don’t know
13. Do you evaluate the following hard tissues status?
- Recontouring of alveolar ridges (alveoplasty) yes No
- Maxillary tuberosity reduction yes No
- Ecostosis yes No
- Removal of tori and undercuts yes No
14. Do you consult oral- maxillofacial specialist for cases with bone or soft tissue defect?
- Yes
- No
- Sometime
15. If you don’t consult oral - maxillofacial surgeon, what will be your line of treatment for cases with the defect.
- You do some surgical procedures
- You refer the patient for expert
- Construct denture even with flat ridge
- Others:….
16. Do you refer for following cases with hard tissues correction for surgery?
- Recontouring of alveolar ridges (alveoplasty) yes No
- Maxillary tuberosity reduction yes No
- Ecostosis yes No
- Removal of tori and undercuts yes No
17. Do you adivce dental implants to reconstruct patient’s complete denture?
- Yes
- No
- According to the patient need and preferences
18. Do you put dental implants to reconstruct patient’s complete denture?
- Yes
- No
- Refer the patient to surgeon for implant insertion
19. If a patient required augmentation of an atrophic maxilla. what method would you prefer to have done?
a. Implant
b. Alloplastic Augmentation
c. Autogenous Bone Grafting
d. No Preference e
e. No Experience
20. If a patient required augmentation of an atrophic mandible, what method would you prefer to have done?
a. Implant
b. Alloplastic Augmentation
c. Autogenous Bone Grafting
d. No Preference e.
e. No Experience
21. What area of the mandibular vestibule do you perceive as the most critical in obtaining maximal depth if a vestibuloplasty is to be performed?
a. Mentalis Region
b. Genioglossal Region
c. Mylohyoid Area
d. Buccal Shelf Area
22. If a vestibuloplasty and graft are to be performed on a patient, which tissue type do you prefer to work with postoperatively?
a. Buccal Mucosa
b. Palatal Mucosa
c. Skin d. No Preference
Citation: Orafi M, et al. (2021). Awareness and Preference of general dental practitioners towards pre-prosthetic surgery as an adjunctive to complete denture therapy. Dental. 3(1):08.
Copyright: Orafi M, et al. © (2021). This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
 Abstract
Abstract  PDF
PDF